Simplified Hypoparathyroidism: A Guide for Nursing & Medical Exams
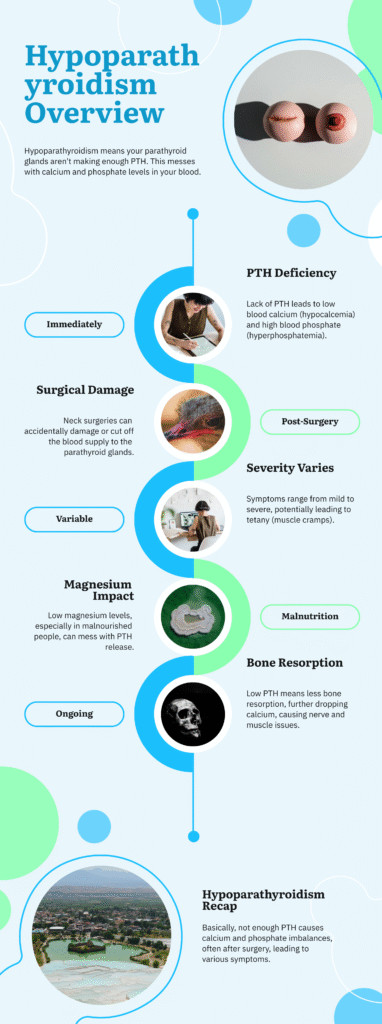
What is Hypoparathyroidism? – A Basic Overview
Hypoparathyroidism refers to a medical condition where there is insufficient production or activity of parathyroid hormone (PTH). This hormonal deficiency leads to low calcium levels (hypocalcemia) and high phosphate levels (hyperphosphatemia), due to reduced PTH action on bones and kidneys. the Epidemiology of hypoparathyrodism is Estimated prevalence is 8–15 cases per 100,000 people globally
Types of Hypoparathyroidism
- Post-Surgical or Acquired Hypoparathyroidism
- Typically occurs due to damage or removal of the parathyroid glands during neck or thyroid surgeries, or as a side effect of radiation or chemotherapy.
- Autoimmune Hypoparathyroidism
- Happens when the body’s immune system mistakenly targets the parathyroid glands or PTH itself.
- Congenital or Idiopathic Hypoparathyroidism
- Present from birth, often linked to genetic defects in PTH production or action.
- Familial Hypoparathyroidism
- An inherited form with no other endocrine or developmental disorders involved.
Causes (Aetiology)
| Treatment-Related Causes (Iatrogenic) | Unknown/Immune Causes (Idiopathic) |
| Removal of parathyroid tissue during thyroid surgeries | Grave’s disease (autoimmune hyperthyroidism) |
| Blood supply loss causing parathyroid infarction | Hashimoto’s thyroiditis (autoimmune hypothyroidism) |
| Scar tissue compressing parathyroid glands post-surgery |
Risk Factors
How It Develops (Pathophysiology)
- Lack of PTH reduces calcium in blood (hypocalcemia) and raises phosphate (hyperphosphatemia).
- Neck surgeries can harm parathyroid glands or restrict their blood supply.
- Severity may range from mild symptoms to tetany (involuntary muscle cramps).
- Low magnesium levels can impair PTH release, especially in malnourished individuals.
- Decreased bone resorption due to low PTH further lowers calcium, leading to nerve and muscle hyperexcitability.
Signs and Symptoms
1. Heart-related:
- Irregular heartbeat
- Bluish skin (cyanosis)
2. Digestive system:
- Nausea, vomiting, abdominal discomfort
3. Skin, Hair, Nails:
- White patches (vitiligo)
- Dry, scaly skin
- Brittle nails with horizontal ridges
- Thinning of hair
4. Nervous system:
- Numbness or tingling (especially around mouth and fingers)
- Trembling, twitching
5. Muscle and Respiratory Symptoms:
- Muscle spasms or cramps
- Hoarseness or difficulty breathing (stridor)
- Facial muscle twitching (Chvostek’s sign)
- Hand spasm during BP cuff inflation (Trousseau’s sign)
6. Other Issues:
- Dental problems
- Eye complications (cataracts, swelling of optic nerve)
How It’s Diagnosed
Clinical History:
- Surgical history (especially thyroid/neck surgeries), symptoms like cramps or numbness, and dietary/alcohol history
Physical Exam:
- Look for signs of low calcium such as positive Chvostek’s and Trousseau’s signs, muscle spasms, and exaggerated reflexes
Lab Investigations:
- High phosphate levels
- Low calcium levels (<7.5 mg/100 ml)
- Low magnesium
- Bone scans may show increased density in chronic cases
Treatment and Management
- Calcium Therapy:
- Oral calcium for maintenance
- IV calcium (calcium gluconate or chloride) during emergencies
- Phosphate Binders:
- Agents like aluminum hydroxide taken after meals to reduce phosphate absorption
- Vitamin D Supplements (Calcitriol):
- Improves calcium absorption and lowers phosphate levels
2 Comments