Hyperparathyroidism Made Easy: Types, Symptoms, and Nursing Management Guide
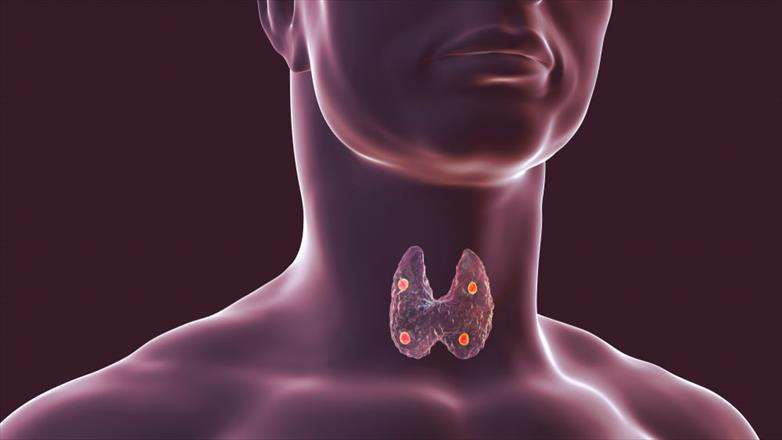
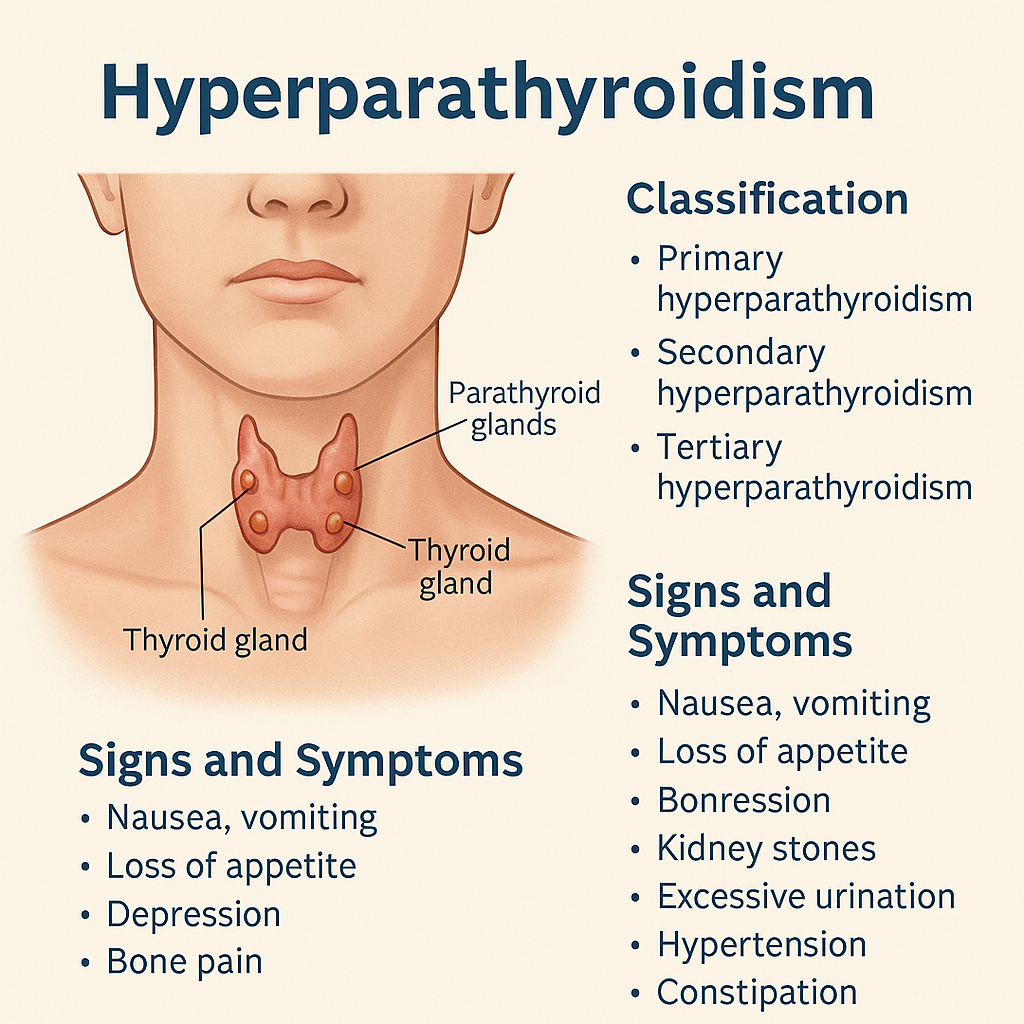
Hyperparathyroidism happens when there is too much parathyroid hormone (PTH) in the blood. This is due to overactivity of one or more (total four) parathyroid glands in the neck.
Types / Classification of Hyperparathyroidism
- Primary Hyperparathyroidism:
This occurs when the normal control between calcium levels and PTH secretion breaks down. It’s more common in women (2 to 4 times) than men. - Secondary Hyperparathyroidism:
Here, the glands become enlarged due to other body problems, like kidney failure. It can happen at any age in kidney patients. - Tertiary Hyperparathyroidism:
In this type, the glands keep making too much PTH even when calcium levels are normal, usually after long-term kidney problems.
Causes (Etiology) of Hyperparathyroidism
| Primary | Secondary | Tertiary |
| • Non-cancerous tumor (adenoma) | • Paget’s disease, bone cancers | • Overactive PTH even when calcium is normal |
| • Growth in two or more glands | • Kidney failure | • After kidney transplant |
| • Cancerous tumors (rare) | • Severe calcium (hypocalcaemia) or vitamin D deficiency | • Long-term secondary hyperparathyroidism |
Risk Factors
- Being female
- Chronic kidney disease
- Past neck or thyroid surgery
- Radiation therapy to the neck
- Lack of calcium or vitamin D in the diet
Pathophysiology
Primary Type:
- Most cases are due to a single gland tumor (adenoma).
- PTH causes calcium to increase in the blood from bones, kidneys, and intestines.
- Bone loss and kidney stones are common.
Secondary Type:
- Kidneys don’t filter properly, leading to high phosphorus and low calcium.
- Low calcium increases PTH production.
- PTH works harder to keep phosphorus under control.
Tertiary Type:
- Parathyroid glands stay overactive even after the original problem (like kidney disease) is treated.
Signs and Symptoms
- Nausea and vomiting
- Loss of appetite
- Depression, tiredness
- Bone pain, joint pain, fractures
- Bone deformities like rickets
- Kidney stones, frequent urination
- High blood pressure
- Constipation
- Mental changes: from anxiety to confusion
Diagnostic Tests
- Medical History: Past surgeries, kidney stones, bone pain
- Physical Exam: Look for signs like high blood pressure
- Ultrasound: Helps locate enlarged parathyroid glands
- CT or MRI: Gives detailed images when ultrasound is not enough
- Urine Test: Checks kidney function
- X-ray: Shows bone damage or thinning
Management and Treatment
Medical (Non-surgical) Treatment
- Primary type: Low-calcium diet
- Secondary type: Calcium supplements and phosphorus restriction
- Hydration: Saline helps flush out extra calcium
- Medications:
- Plicamycin (a rare antibiotic for lowering calcium)
- Bisphosphonates (to prevent bone loss)
Surgical Treatment
- Most common and effective for primary type
- Surgeon removes one or more overactive glands
- If all four are affected, only 3 or part of the 4th gland is removed
- Usually outpatient surgery with small neck incisions
- Risks:
- Vocal cord nerve damage
- Long-term low calcium (needs supplements)
Complications of Hyperparathyroidism:
- Kidney Stones (Nephrolithiasis)
- Osteoporosis
- Renal Impairment or Chronic Kidney Disease (CKD)
- Peptic Ulcers and Pancreatitis– Hypercalcemia stimulates gastric acid secretion and may trigger inflammation in the pancreas.
- Arrhythmias (Irregular Heartbeats)
Nursing Care Plan
- Ask patient about symptoms like bone pain or fatigue
- Monitor calcium levels and vital signs
- Encourage a balanced diet
- Provide prescribed supplements
- Help with walking or movement if bones are weak
- Ensure bed safety
- Give small, frequent meals
- Encourage fluids
- Assist with hygiene and oral care