HYPOKALAEMIA: How to treat and manage
What is hypokalaemia?
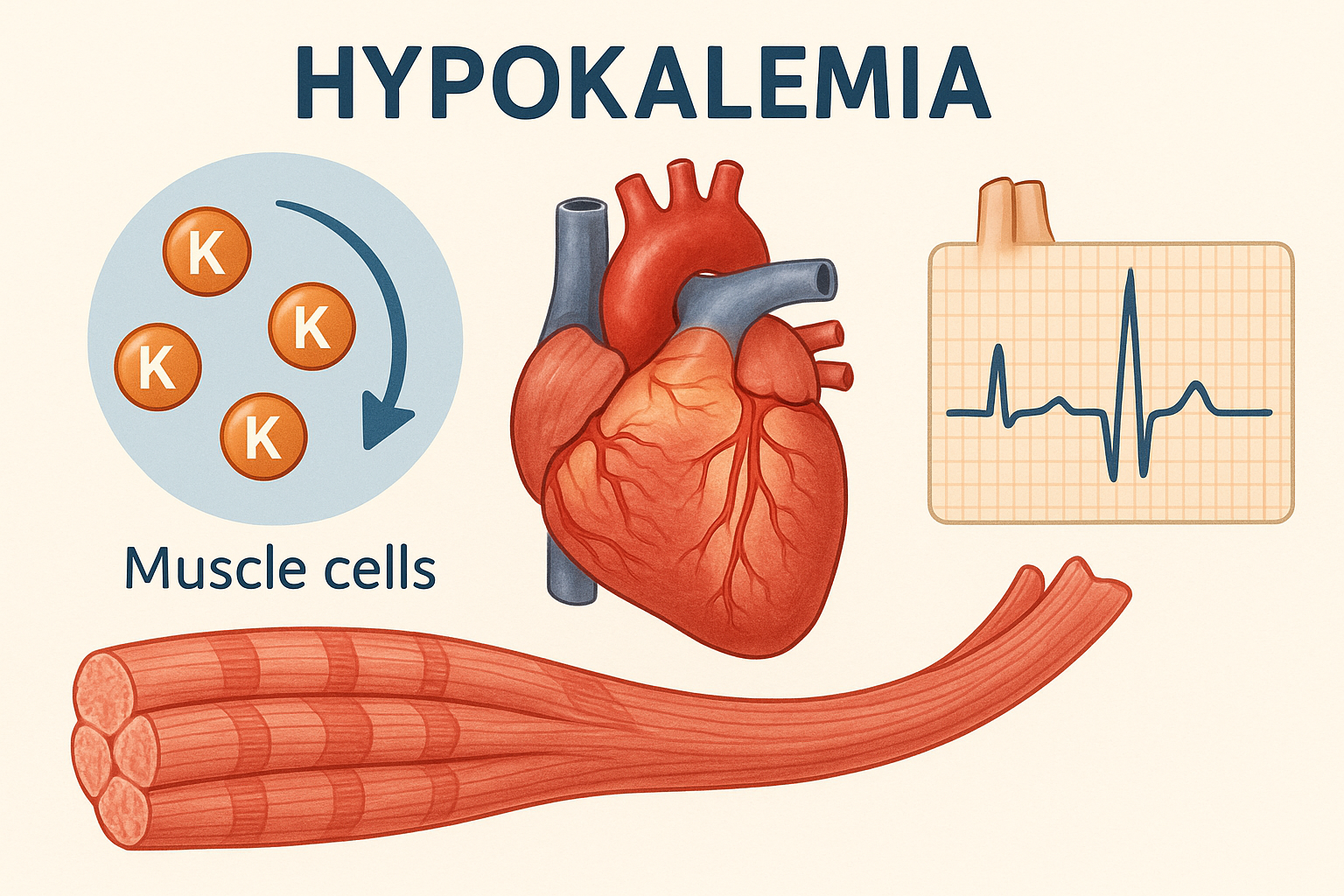
Hypokalaemia is a condition which is characterized by a lower-than-normal level of potassium in the blood. The serum potassium concentration is below or less than 3.5 mmol/L (normal range: 3.5–5.0 mmol/L).
- Potassium is a vital electrolyte, with about 98% found inside the body’s cells. It helps maintain the electrical balance across cell membranes, which is especially important for proper muscle and nerve function.

Types of hypokalaemia
- Mild hypokalaemia- The serum potassium concentration is (3.0–3.5 mmol/L).
- Moderate hypokalaemia- The serum potassium concentration is (2.5–3.0 mmol/L).
- Severe hypokalaemia-The serum potassium concentration is (less than 2.5mmol/L).
| Severity | Potassium Level (mmol/L) | Symptoms | Treatment |
| Mild | 3.0-3.5 | Often none, mild | Dietary changes, oral supplements |
| Moderate | 2.5-3.0 | Muscle weakness, cramps | Oral/IV supplements, treat cause |
| Severe | Less than 2.5 | Arrhythmias, paralysis | IV supplements, urgent care |
Causes of hypokalaemia
- Increased Loss of Potassium (Most Common)–
- Gastrointestinal losses: vomiting, diarrhoea, chronic laxative use, intestinal obstructions.
- Renal losses: diuretics (especially loop and thiazide), osmotic diuresis (diabetes mellitus), mineralocorticoid excess (Cushing’s syndrome), other renal tubular disorders
- Medications: corticosteroids (Corticosteroids cause hypokalaemia by increasing renal potassium excretion through enhanced sodium reabsorption via activation of mineralocorticoid receptors.), some antibiotics, amphotericin B, insulin overdose.
- cellular Shifts–
- Alkalosis (potassium moves into cells)
- Insulin administration (drives potassium into cells)
- Beta-adrenergic stimulation (activation of the Na⁺/K⁺-ATPase pump)
- Hypokalaemia periodic paralysis (rare genetic disorder causing episodic potassium shifts into cells)
- Refeeding syndrome (potassium shifts into cells during carbohydrate refeeding in malnourished patients)
- Inadequate Intake–
- Starvation
- Anorexia
- Eating disorders
- Malnutrition
- Excessive Sweating–
- Loss through sweat, especially in hot weather or extreme exercise
Pathophysiology of hypokalaemia
Potassium is essential for maintaining the resting membrane potential in cells, especially in heart and skeletal muscles.
When potassium levels drop (hypokalemia), the following changes occur:
- Cell membranes become hyperpolarized, meaning it’s harder for them to activate.
- This leads to reduced nerve and muscle activity, causing weakness or cramps.
- The abnormal electrical activity slows or disrupts nerve signals, increasing the risk of dangerous heart rhythm problems (arrhythmias).
- In severe cases, the sodium-potassium pump (Na⁺/K⁺-ATPase), which helps maintain fluid and electrolyte balance in cells, becomes impaired — affecting overall cell function and stability.
Clinical Features of hypokalaemia
- Often Asymptomatic (especially if develops slowly).
Neuromuscular Symptoms
- Muscle Weakness: Often begins in the legs and is caused by changes in the muscle cell membrane potential.
- Muscle Cramps and Aches (Myalgias): Result from impaired muscle excitability.
- Paralysis: May occur in severe cases, such as in hypokalaemic periodic paralysis, where muscle function is temporarily lost.
- Rhabdomyolysis (muscle breakdown): A rare but serious complication due to prolonged reduced blood flow and oxygen to muscles in extreme hypokalemia.
Cardiovascular Effects
- Arrhythmias (Abnormal Heart Rhythms):
- Early beats from the atria or ventricles (PACs or PVCs).
- Dangerous rhythms like ventricular tachycardia or ventricular fibrillation.
- Torsades de Pointes: A specific life-threatening rhythm, especially if low magnesium is also present.
- ECG (Electrocardiogram) Changes:
- Flattened or inverted T waves
- Prominent U waves, especially in chest leads.
- ST-segment depression
- Prolonged QT interval, which raises the risk of serious arrhythmias.
- Hypertension (High Blood Pressure):
- May occur if hypokalemia is caused by excess aldosterone or similar hormones (e.g., in Conn’s syndrome).
Gastrointestinal Symptoms
- Ileus (Paralysis of the Gut): Caused by decreased activity of smooth muscles in the intestines, leading to reduced bowel movement.
- Constipation: Due to sluggish intestinal motility.
- Nausea: Often occurs when hypokalemia is linked with alkalosis or frequent vomiting.
Renal (Kidney) Effects
- Polyuria (Excessive Urine) and Polydipsia (Excessive Thirst):
Low potassium reduces the kidneys’ ability to concentrate urine, leading to a condition similar to nephrogenic diabetes insipidus. - Metabolic Alkalosis:
Long-term hypokalemia causes the kidneys to excrete more hydrogen ions (H⁺), leading to a rise in blood pH (alkalosis).
Respiratory Effects:
- Respiratory muscle weakness: Rare, in severe cases, leading to hypoventilation.
Diagnosis of Hypokalaemia
- Blood Tests:
Confirm low serum potassium levels (< 3.5 mEq/L). - Electrocardiogram (ECG):
May reveal characteristic changes such as:- Flattened or inverted T waves
- Prominent U waves
- ST-segment depression
- Arrhythmias, particularly in severe hypokalaemia
- Clinical Assessment:
Identify the underlying cause by evaluating:- Medical history (e.g., vomiting, diarrhea, diuretic use)
- Medication review
- Renal and gastrointestinal losses
- Associated conditions (e.g., hyperaldosteronism, eating disorders)
- Urinary potassium:
- Spot urine potassium:
- <20 mEq/L: Suggests extrarenal losses (GI loss) or cellular shifts.
- Spot urine potassium:
- Imaging (If Indicated)
- Adrenal Imaging (CT or MRI):
Performed when Conn’s syndrome (primary hyperaldosteronism) or adrenal tumors are suspected as the cause of hypokalemia. - Renal Ultrasound:
Used to detect structural abnormalities in the kidneys that may contribute to potassium loss.
- Adrenal Imaging (CT or MRI):
Treatment
General Management Principles for Hypokalaemia
1. Correct Coexisting Electrolyte Abnormalities
- Fix low magnesium first if present, as it can make potassium correction difficult (refractory hypokalemia).
2. Monitoring Guidelines
- Serum Potassium: Check every 4–6 hours during active repletion.
- ECG Monitoring: Watch for arrhythmias or changes in T/U waves.
- Cardiac Monitoring: Required if potassium is <2.5 mEq/L or patient has arrhythmias.
3. Avoid Rapid Correction
- Risk: Overcorrection may lead to hyperkalaemia (dangerously high potassium).
- IV Rate Limit:
- 10–20 mEq/hour (typical safe range)
- Up to 40 mEq/hour only in life-threatening cases with cardiac monitoring
- Maximum Peripheral IV Concentration: ≤40 mEq/L
- Central Line Use: Required for concentrations >40 mEq/L
Potassium Repletion Methods
A. Oral Repletion (Preferred for Mild to Moderate Cases)
Indications: Serum K⁺ between 3.0–3.5 mEq/L in stable patients
- Potassium chloride (KCl): Most commonly used, especially with alkalosis
- Potassium citrate or bicarbonate: Preferred if metabolic acidosis (e.g., renal tubular acidosis)
- Potassium phosphate: For patients with low phosphate (e.g., in refeeding syndrome)
- Typical Dose: 20–40 mEq every 4–6 hours, adjusted by lab response
- Note: High-potassium foods (bananas, oranges, potatoes) help long-term but are not effective for rapid correction.
B. Intravenous (IV) Repletion
Indications: Severe hypokalemia (<2.5 mEq/L), symptomatic patients, or those unable to take oral potassium
- Formulation: KCl in normal saline
- Avoid Dextrose: It increases insulin and worsens hypokalemia
- Peripheral IV: ≤40 mEq/L to prevent vein irritation
- Central Line: Needed for higher concentrations (up to 80 mEq/L)
- Estimated Total Dose:
- For each 0.1 mEq/L drop in potassium → ~100–200 mEq of K⁺ may be required
4. Treat the Underlying Cause
A. Discontinue or Adjust Offending Drugs
- Examples: Diuretics (loop/thiazide), laxatives, beta-agonists
B. Replace Losses
- GI Losses: Use IV fluids and electrolytes to replace vomiting/diarrhea losses
C. Hormonal Imbalances
- Mineralocorticoid excess (e.g., Conn’s syndrome):
- Use spironolactone or eplerenone
- Surgical removal of adrenal tumor if needed
D. Renal Disorders
- Bartter or Gitelman syndromes:
- Use potassium-sparing diuretics (e.g., amiloride)
- Supplement with magnesium
E. Transcellular Potassium Shifts
- Correct metabolic alkalosis (e.g., with volume repletion)
- Monitor insulin and beta-agonist therapies that may push K⁺ into cells
Potassium-Sparing Strategies
- Amiloride / Triamterene: Block sodium reabsorption, reducing potassium loss
- Spironolactone: Blocks aldosterone
- ACE Inhibitors / ARBs: Lower aldosterone production, especially in secondary hyperaldosteronism
Ongoing Monitoring
- Repeat serum potassium levels frequently during correction
- Watch for overcorrection (hyperkalemia):
- ECG signs: Peaked T waves, bradycardia, etc.
- Check kidney function: Poor renal function may require dose adjustments
You can also read-