IRON DEFICIENCY ANAEMIA- simple ways to prevention
Iron deficiency anaemia
Definition
Iron deficiency anaemia is the most common cause of anaemia where too little iron and ↓ Haemoglobin level in the body which leads to ↓ Oxygen delivery to tissues.
It is the most common anaemia worldwide
Anatomy & Physiology
- Iron absorbed mainly in the duodenum part of the small intestine.
- Iron is required to make haemoglobin which help to make RBC.
- RBC life span = 120 days
Causes of Iron Deficiency Anaemia
1. Increased Iron Loss (MOST COMMON)
- Heavy menstrual bleeding
- GI bleeding (ulcer, hemorrhoids, cancer)
- Hookworm infestation
2. Inadequate Intake
- Poor diet intake.
- Malnutrition individual.
- Unplanned vegetarian diet
3. Increased Demand
- Pregnancy
- Lactation
- Infancy & adolescence
4. Malabsorption
- Celiac disease
- Post-gastrectomy
Pathophysiology of iron deficiency anaemia
Poor dietary intake / Poor absorption / Increased demand / Chronic blood loss
↓
Decreased iron availability in the body
↓
Depletion of iron stores (liver, spleen, bone marrow)
↓
Insufficient iron for haemoglobin synthesis
↓
Decreased haemoglobin production
↓
Impaired red blood cell production in bone marrow
↓
Formation of microcytic, hypochromic red blood cells
↓
Reduced oxygen-carrying capacity of blood
↓
Decreased oxygen delivery to tissues
↓
Tissue hypoxia
Clinical Manifestations
General Symptoms
- Fatigue
- Weakness
- Dizziness
- Headache
Skin & Nails
- Pallor
- Brittle nails
- Spoon-shaped nails (koilonychia)
Oral Changes
- Glossitis (smooth red tongue)
- Angular stomatitis
Pica
- Craving ice, clay, starch, chalk
Remember– Pica + pallor + fatigue = iron deficiency anaemia
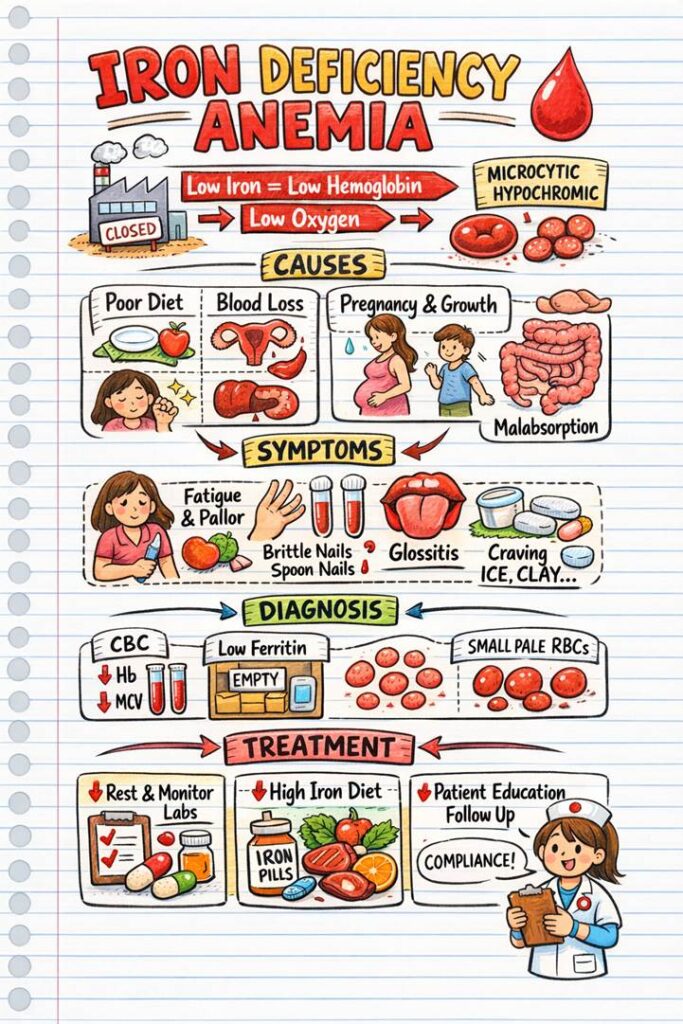
Diagnostic Evaluation
1. CBC
- ↓ Haemoglobin
- ↓ Haematocrit
- ↓ MCV (microcytic)
2. Iron Studies
| Test | IDA Result |
| Serum iron | ↓ |
| Ferritin | ↓↓↓ |
| TIBC | ↑ |
| Transferrin saturation | ↓ |
Remember- Ferritin = best indicator of iron stores
3. Peripheral Blood Smear
- Small, pale RBCs
Medical Management
Oral Iron Therapy (First Line)
- Give Ferrous sulphate / fumarate / gluconate
iron and folic acid (IFA) therapy
| Population | Purpose | Iron Dose (elemental) | Folic Acid Dose | Frequency | Notes / Source |
|---|---|---|---|---|---|
| Children (6–59 months) | Prevention (public health) | 20 mg | 100 mcg | Biweekly | NIPI / national programme for school/adolescents; age-specific syrup dosing for younger children (National Health Mission) |
| Children (6–59 months) – Treatment of IDA | Treatment | 3–6 mg/kg/day | Not usually specific unless folate deficiency suspected | Daily | Clinical approach (3–6 mg/kg/day elemental iron) (Royal Children’s Hospital) |
| Children (5–10 years) | Prevention | 45 mg | 400 mcg | Weekly | NIPI / national programme (National Health Mission) |
| Children & Adolescents (10–19 years) | Prevention | 100 mg | 500 mcg | Weekly | NIPI / national programme (National Health Mission) |
| Adults (non-pregnant) – prophylaxis/treatment | Treat diagnosed IDA | 60–120 mg (often 60–100 mg) | 400 mcg | Daily | WHO’s recommended daily IFA for women/fair for adults; clinical treatment varies with severity (World Health Organization) |
| Pregnant Women – prophylaxis (WHO) | Prevent maternal anemia | 30–60 mg | 400 mcg (0.4 mg) | Daily | WHO daily supplementation recommendation (World Health Organization) |
| Pregnant Women – prophylaxis (India/NIPI) | Prevent anemia in pregnancy | 100 mg | 500 mcg | Daily for ≥100 days | National programme (starting ~14–16 weeks gestation) (National Health Mission) |
| Pregnant Women – treatment of IDA | Treat iron deficiency anemia | 120 mg | 400 mcg | Daily until Hb normalizes | Clinical guideline for anemia treatment (NCBI) |
| Older Adults (>60 years) – treatment | Treat diagnosed IDA | 60–120 mg (as tolerated) | 400–600 mcg | Daily | No specific guideline: clinical practice uses adult doses adjusted based on tolerance and comorbidity (ScienceDirect) |
Nursing Teaching
- Take on empty stomach if tolerated
- Take with vitamin C
- Avoid milk, tea, antacids
- Black stools are normal
- Constipation common
- Continue iron 3–6 months after Hb normalizes
Parenteral Iron
Used when:
- Oral iron not tolerated
- Malabsorption
- Severe deficiency
Note- Monitor for allergic reactions
Blood Transfusion
- Only for severe or life-threatening anaemia
Dietary Management
1. Iron-Rich Foods
2. Heme Iron (Best absorbed):
- Red meat
- Liver
- Fish
3. Non-Heme Iron:
- Spinach
- Beans
- Lentils
- Dates
- Jaggery
4. Improves Absorption
- Vitamin C (orange, lemon)
5. Decreases Absorption
- Tea
- Coffee
- Milk
Nursing Care Plan (NCP) –
NCP 1: Fatigue
Related to: Decreased oxygen-carrying capacity
Evidenced by: Weakness, lethargy
Goals:
- Improved energy
- Able to perform ADLs
Interventions:
- Schedule rest periods
- Assist with activities
- Monitor Hb & ferritin
NCP 2: Imbalanced Nutrition
Related to: Inadequate iron intake
Interventions:
- Educate on iron-rich diet
- Encourage vitamin C intake
- Dietitian referral
NCP 3: Activity Intolerance
Related to: Reduced oxygen delivery
Interventions:
- Gradual activity increase
- Monitor HR & SpO₂
- Stop activity if dyspnoea occurs
NCP 4: Knowledge Deficit
Related to: Iron therapy
Interventions:
- Explain long duration of therapy
- Teach side effects
- Stress adherence importance